New computational system for measuring heart's blood flow after percutaneous coronary intervention
The authors of this work created a computational mechanism to calculate blood flow in a coronary artery, a very important step in the restoration of blood flow after a myocardial infarction.
Myocardial infarction follows from a reduction in blood flow (perfusion) at an specific heart area due to the obstruction (total or partial) of one of the coronary arteries irrigating it. A common clinical treatment for blood flow restoration consists in opening the affected artery by percutaneous coronary intervention. In a high percentage of interventions, a proper restoration of arterial flow does not always correlate with adequate myocardial perfusion due to microcirculation obstruction.
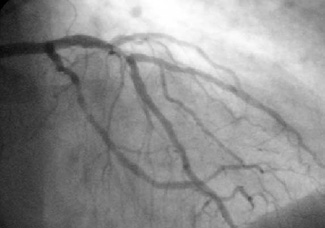
In the last years, several diagnosis techniques to assess the degree of the restored perfusion have been developed. One of the most extended is assessment of the myocardial staining observed in contrast angiography. Such degree of staining is currently visually assessed and requires of a highly expertise for its reliable determination. In this work, we present a computational tool which, by means of image processing techniques, allows objective quantification of the myocardium opacification in contrast angiography sequences.
Figure 1a. The signal obtained is the contribution of four main phenomena: arterial staining, myocardial staining, breathing and radiological noise.
The microcirculation contrast absorption can be detected by changes in the image gray-values (intensity) along the angiographic sequence. The evolution of the image local mean (LM) provides, for each pixel, a graphic which reflects the amount of contrast absorbed at each point. The signal obtained is the contribution of four main phenomena: arterial staining, myocardial staining, breathing and radiological noise (Fig.1). The two latter, especially breathing, are a main artifact that might distort the staining pattern.
Figure 2a. Descriptors proposed: Maximum staining (amplitude of the Fourier coefficient, Imax) and time such maximum is achieved (phase of the Fourier coefficient, tImax).
Given that each phenomenon has a distinctive repetition pattern (frequency), we have used Fourier analysis for decoupling them. Myocardial staining is a phenomenon that happens only once along the sequence and thus it is given by the frequency 1 of LM Fourier development. The descriptors we propose (Fig.2a) are the maximum staining (amplitude of the Fourier coefficient, Imax) and time such maximum is achieved (phase of the Fourier coefficient, tImax). The representation of these values for all image pixels (Fig.2b) describes the
myocardial staining pattern: arterial staining (A), myocardial staining (M) and noise (N).
Figura 2b. The representation of these values for all image pixels describes the myocardial staining pattern: arterial staining (A), myocardial staining (M) and noise (N).
Experiments were designed to address the reliability of the descriptors for determining the degree of staining and breathing influence. A total number of 20 sequences of right coronary arteries without apparent lesions with the patient breathing and in breath-hold (apnea) were analyzed. We consider that (Imax, tImax) properly describe the staining pattern if their values characterize and discriminate the 3 staining phenomena A, M and N.
Our statistical analysis indicates that there are not significant differences between results obtaining in apnea and with the patient normally breathing. Regarding the capability for myocardial staining quantification, we have a sensibility and specificity over 95%. Therefore the proposed descriptors might be used in systematic clinical practice for an objective assessment of myocardial perfusion in infracted patients undergoing percutaneous coronary intervention.
References
"Myocardial perfusion characterization from contrast angiography spectral distribution". Gil, Debora; Rodriguez-Leor, Oriol; Radeva, Petia; Mauri, Josepa. IEEE TRANSACTIONS ON MEDICAL IMAGING, 27 (5): 641-649 MAY 2008.

